How new technology aims to lower carbon emissions and improve patient health at UC San Diego Health
The healthcare industry is increasingly clear-eyed about the impacts of climate change on its ability to provide patient care and its responsibility to reduce greenhouse gas emissions. An editorial in the New England Journal of Medicine labeled climate change “a health emergency,” noting that a warming world challenges the work of doctors and nurses in numerous ways—from the need to treat people injured or sickened by extreme weather events to a rise in infectious diseases to the psychological impacts of wildfires, droughts, hurricanes, air pollution, and other negative consequences of climate change.
“Working to rapidly curtail greenhouse gas emissions is now essential to our healing mission,” wrote the editorial’s authors. The need to decarbonize the healthcare industry is particularly important because hospitals, clinics, medical equipment manufacturers, supplies, and pharmaceuticals are major contributors to greenhouse gas emissions. A study published in HealthAffairs found that the U.S. healthcare industry was responsible for 8.5 percent of America’s total carbon footprint.
These emissions are also on the upswing. A report released last year by the nonprofit organization Health Care Without Harm noted that the industry’s global emissions could triple by 2050 without major changes. Health Care Without Harm is one of numerous organizations—including the National Academy of Medicine and the American College of Physicians—that have formulated aggressive strategies to decarbonize.
There are already numerous tools and technologies that organizations in the healthcare sector can utilize to drive down greenhouse gas emissions. For example, California-based health system Kaiser Permanente announced in 2020 that it had achieved carbon neutrality through measures such as improving energy efficiency and installing on-site renewable energy at its facilities and purchasing carbon-free electricity from external suppliers and carbon credits to offset emissions.
The Need for Innovation
Healthcare decarbonization requires technology innovation to reduce the amount of energy hospitals, and clinics use while still meeting stringent indoor air quality requirements. But emerging and potentially beneficial technologies face a challenge: they must first be vetted and tested in real-world conditions before achieving the scale that will have a significant impact.
One of EPRI’s primary roles is to facilitate projects that test and evaluate promising new technologies. “When EPRI gets its hands on emerging technologies, we run field trials and try to validate the technology or the market,” said Agatha Kazdan, an EPRI principal technical leader. “We are trying to look at it from the state’s and utilities’ perspectives to verify how this improves the situation for society, ratepayers, and operation of the grid.”
A new project at Jacobs Medical Center at UC San Diego Health aims to confirm the decarbonization and other benefits a promising cooling and dehumidification technology can deliver in a healthcare setting. The project, which is supported by a $1.44 million grant from the California Energy Commission (CEC) and is being implemented and evaluated by EPRI, involves the installation of two high-efficiency dehumidification system (HEDS) air handling units (AHUs) designed by Conservant Systems, Inc. to serve seven operating rooms and the associated support spaces at Jacobs Medical Center.
“The HEDS technology has the potential to decarbonize large commercial buildings, like healthcare facilities, in an energy-efficient way by reducing energy use and greenhouse gas emissions while providing benefits to the electric grid and providing building occupants with a healthy and comfortable environment,” said Jonah Steinbuck, director of the Energy Research and Development Division at the CEC.
The Importance of Air Quality at Healthcare Facilities
One driver of interest in HEDS technology is its potential to address both current and future challenges faced by healthcare heating, ventilation, and air conditioning (HVAC) systems. An increasing concern is how to properly control relative humidity as the world becomes warmer and wetter.
Many of the HVAC systems used in healthcare facilities today were designed and built 20 to 40 years ago. “They were never designed to work with today’s outdoor conditions,” EPRI’s Kazdan said. “Equipment wear and performance degradation can also create conditions that promote the growth and spread of biological pathogens and healthcare-associated infections (HAIs).”
HEDS can both cool and dehumidify buildings while also filtering the air to reduce the spread of biological pathogens and viruses like COVID-19. The systems will replace UC San Diego Health’s existing AHUs, which rely on chillers and boilers powered by both electricity and natural gas to control the temperature and relative humidity of indoor environments. Replacing the existing AHUs with significantly more efficient HEDS is expected to reduce the energy consumption required by boilers and chillers. In non-healthcare Department of Defense (DoD) and federal laboratory applications, the HEDS technology has been shown to reduce the cooling and heating loads for temperature control and dehumidification by over 50 percent and requires very little maintenance.
The potential of the new HEDS units to simultaneously lower emissions and costs while ensuring operating rooms maintain the optimal temperature and relative humidity was an important driver of the project. “In operating rooms, the surgeons and patients are in a critical state during surgery,” Kazdan said. “The value proposition was energy savings and reducing operating costs and emissions. But it’s also improving the system’s performance to benefit patients and medical staff.”
Securing benefits for patients was a big reason Joe Dizon, energy manager at UC San Diego Health, was eager to implement the HEDS AHUs. “Humidity and temperature control in operating rooms is critical to patient safety, which is our first priority,” Dizon said. “The new units will better serve our facilities by improving the air quality. This, in turn, supports a safer environment for patients and does so more efficiently. Being able to both increase patient safety and decrease energy usage directly aligns with the goals of our organization.”
Part of a Larger Decarbonization Effort
It’s also important to keep in mind the broader context surrounding this project, particularly as it relates to decarbonization. California recently passed legislation to achieve 90 percent zero-carbon electricity by the end of 2035 as part of the state’s commitment to achieving economy-wide net-zero emissions by 2045.
The University of California also has ambitious climate and energy goals. For example, the UC system as a whole has pledged to use 100 percent clean electricity by 2025 and achieve Scope 1 and Scope 2 climate neutrality in the same year. In addition, UC campuses and health facilities have targeted a 2 percent annual reduction in energy use intensity. The UC system’s multibillion-dollar endowment and pension funds have also divested all fossil fuel investments and have financed over 1.7 gigawatts of wind, solar, and battery storage installations around the globe.
UC San Diego Health engages staff, faculty, and leadership across the health system to increase sustainable behaviors that contribute to emissions reductions and community health. Planning efforts are underway to redevelop the system’s medical center in Hillcrest, and construction has begun on a new outpatient pavilion that is designed to reduce carbon intensity by over 90 percent.
Green certification programs for medical clinics, units, and offices provide standardized methods to evaluate, enhance, and recognize sustainable work behaviors and practices. Efforts to improve the sustainability of UC San Diego Health operating rooms have focused on reducing waste, reducing the impacts of anesthetic gas, and improving energy power-down strategies. Procurement strategies have vastly increased the use of energy-efficient electronics and reprocessed single-use devices in trauma operating rooms, which has yielded annual savings of over $800,000 and eliminated nearly 14,000 pounds of waste.
The medical center hosted an initial two-part Climate Resiliency Workshop in partnership with the UC San Diego academic campus. UC San Diego Health is the only medical center in the San Diego region that has joined the UN Race to Zero climate commitment.
How HEDS Work
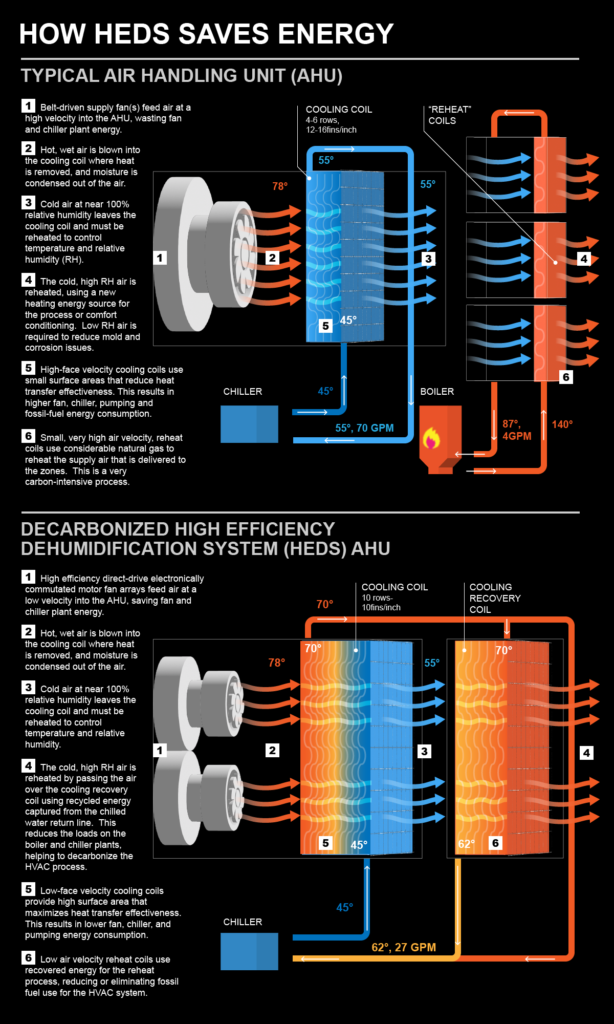
Grasping how HEDS work is necessary to understand how a change in the technology used to cool and dehumidify buildings can potentially achieve substantial cost and emissions reductions. At a very basic level, all AHUs are outfitted with heat transfer coils that have hot and cold water running through them. Fans move air across the units, and cold or hot coils cool or heat the air, depending on the needs of the building occupants.
Most AHUs use a lot of energy to do their job. “In most buildings across America, they have what’s called a cooling coil in the unit, and then they have a reheat coil that is above the space where you’re doing your work in the room,” said Chris Roman, director of business development at Conservant Systems, the inventor of HEDS and a partner in the UC San Diego Health project. “If it’s an operating room and you’re a surgeon doing open heart surgery, there’s a coil above your head that heats the space to control relative humidity. It works, but it’s a very, very energy-intensive process.”
A big reason traditional AHUs are so energy intensive is that the cooling and reheating coils have separate energy sources. A chiller powers the cooling coil, and a natural gas boiler creates hot water for the reheat coil.
By contrast, with HEDS, a chiller alone can provide energy to both cooling and reheat coils and meet most of the reheat needs. The reason: the coils in HEDS are designed to capture heat generated during cooling and dehumidification and repurpose that heat rather than wasting it. The reheat coil is supplied with energy already produced, which significantly improves efficiency.
“We reheat the air with the energy we’ve already paid for. So, during surgery, that causes the reheat coil to open very minimally,” Roman said. “The more that reheat coil stays closed, the more load you are removing and the more you are decarbonizing the facility.”
Potential Statewide Impact
HEDS can potentially deliver significant benefits to healthcare facilities across California and the world. EPRI estimated the cost, greenhouse gas emissions, peak load, and water savings benefits that could result if HEDS were used to cool and dehumidify California’s 112 million square feet of healthcare facilities.
For example, EPRI calculated that wide-scale deployment of HEDS could reduce the cooling load at California healthcare facilities by 24 percent and lower annual cooling costs by $26.2 million. HEDS could also significantly reduce peak load, which is particularly important in California, given the strain on the grid due to extreme heat.
Considering the ambitious decarbonization objectives of the state and the university system, the greenhouse gas emissions reductions HEDS can provide are a priority. The emissions reductions result from both improving cooling efficiency and eliminating the use of natural gas for reheating. EPRI estimates that the improved cooling efficiency HEDS provides could reduce CO2 emissions for commercial customers in the state by nearly 800,000 tons.
Eliminating the need for natural gas to fuel reheating in traditional AHUs could reduce commercial reheating emissions reductions of more than four million tons. EPRI also calculated that HEDS technology has a 30 percent lower water evaporation rate than typical AHUs, an important benefit in the drought-stricken state.
Implementation Informed by a Track Record
The implementation of HEDS at UC San Diego Health is an important step in demonstrating and verifying its benefits in a demanding healthcare setting. In turn, this project rests on successful operation of HEDS in other environments since 2016.

The technology was originally developed for the DoD, whose main priorities were maintaining air quality in its facilities and utilizing cooling and dehumidification systems that required little maintenance. “The DoD has very limited maintenance budgets and staffing, so the HEDS was designed to be the lowest lifecycle cost available, with very limited maintenance requirements,” said Scot Duncan, president of Conservant.
As Conservant refined the design, it worked with the U.S. Army and Navy on Guam. “We learned so much about what works and does not work on Guam, and we have upgraded HEDS components to live in that harsh climate so that HEDS can operate in less stressful environments for a long time,” Duncan said.
HEDS have since been used at U.S. Navy, Air Force, and Army facilities, as well as at a government laboratory in San Juan, Puerto Rico. HEDS have performed well enough that the DoD recommended expanded use of the technology in its 2019 High Performance and Sustainable Buildings report to Congress. HEDs were also implemented at the Naval Weapons Station in Seal Beach, California—a project recognized with a 2021 Secretary of the Navy Energy Award in the Technology Development category. HEDS is also being piloted by the U.S. General Services Administration (GSA) as part of an initiative to test and validate building decarbonization technologies.
More recently, HEDS technology was incorporated into a renovation of the Timken Museum in San Diego, with the goal of delivering 99.99 percent purified air and, ultimately, fully electrifying and decarbonizing the HVAC system.
The design phase of the UC San Diego Health project is now complete, and construction is expected to begin by 2024. Once the two HEDS units are finished, EPRI will monitor their performance for a minimum of nine months.
“If the HEDS technology affects healthcare in the same manner that it has worked for the DoD, the federal lab, and the Timken Museum, it could be a game changer from an energy, decarbonization, and HAI-reduction perspective,” Duncan said.
EPRI Technical Expert:
Agatha Kazdan
For more information, contact techexpert@eprijournal.com.